leadership
THOUGHT
By Cory Worden

Missed opportunities, part two
How the fight against COVID-19 became a stalemate
“I want the war to end as quickly as anybody wishes, but I don’t want the nucleus of another war left whole.” – David Webster (Ambrose, 1992).
hen David Webster wrote the above statement, he was an airborne infantry soldier writing home to his parents from France in July 1944 and was referring to World War II. His point was, although his parents wanted an expeditious surrender from Adolf Hitler, Webster was accepting of an extended war effort with the condition that it completely removes the threat of another war. His fear was, should the war end too quickly, the possibility would exist that the Nazis could regroup and attempt to re-start the war.
What the world is countering now in 2021 is not a war and it is not a human enemy. Instead, the world is countering COVID-19, a severe acute respiratory virus, and its variants. The virus is not countered by battle formations and bullets, but instead vaccinations and exposure prevention protocols such as social distancing; teams are protected with respirators and gloves instead of steel helmets.
However, an incomplete success against this viral enemy can also result in its continual return. Since the virus emerged in the United States at the end of January 2020, enormous progress has been made in epidemiology, testing, vaccinations, and exposure prevention. Unfortunately, with many having actively protested exposure prevention protocols since the emergency of the virus and many actively protesting vaccinations, methods to counter the virus are being bypassed by a large percentage of the population; in turn, this is enabling the possibility for COVID-19 to linger and/or return. If a point is reached at which COVID-19 is continuing to circulate but vaccinations are not being received and exposure prevention methods are not being enacted, a stalemate will be reached; the ‘war’ is not won but there is nothing to use against it.
W
Situation report
To summarize the current state of the COVID-19 pandemic (CDC, 2021)(HHD, 2021):
1. There is a clear population divide between those vaccinated and those unvaccinated. In an example of a major city, 53% are fully vaccinated while 47% are unvaccinated. Among the vaccinated, there are 6% more with the first dose but not the second (59% at least partially vaccinated versus 41% unvaccinated). The highest rates of vaccinations are among the 60+ (90% fully vaccinated, 99% partially vaccinated, and 1% unvaccinated).
2. The difference between the infection rates from July 2020 (~21% in an example of a major city) and July 2021 (<5%, but with few consistently coming for testing) is from vaccinations and exposure prevention (source control, capacity limits, social distance, air circulation, barriers, hand hygiene, surface disinfection and/or PPE and respirators).
3. The current infection rate is <5%, but this is with few coming for testing. This means most known cases are severe enough for hospitalization. Most cases are unvaccinated. ~10% are the Delta variant, but the available vaccines are known to be effective against the COVID-19 variants. Outbreaks are still occurring among the unvaccinated. The ~5% vaccine inefficacy risk also presents a small risk of transmission. Infection numbers increased in all 50 states lately.
4. In short, vaccinations provide a good level of protection and COVID 19 is still circulating, mainly affecting the unvaccinated. If unvaccinated, exposure prevention methods such as social distance, avoiding large indoor crowds, and hand hygiene are good for preventing infections until the hazard and risk reduce. Face masks only serve for droplet containment (source control) that helps others (unvaccinated or the ~5% vaccine inefficacy risk). If unvaccinated and not enacting exposure prevention, the risk is around 1 in 20 or lower and with possibly heightened severity.
5. The key to risk reduction is to reduce frequency and severity. Frequency is reduced through vaccinations or exposure prevention (the fewer vulnerable hosts and the fewer infections and exposures, the virus stops circulating). Severity is reduced through vaccinations and medical treatment.
6. Without vaccinations or exposure prevention, the virus keeps circulating and will only stop through nature or luck. If it keeps circulating, the unvaccinated (especially without exposure prevention) and the ~5% vaccine inefficacy risk are at risk.
The risk assessment
As the Center for Disease Control (CDC) announced new guidance in May 2021 that those with complete COVID-19 vaccinations may begin relaxing exposure prevention protocols, the occasion could have been interpreted as a milestone in the then-20-month trajectory of the global COVID-19 pandemic, a victory of sorts. However, two factors prevented this from being the victory it should have been:
1. A significant percentage of the population is not vaccinated as of July 2021, even with vaccines available to them. This is not to judge anyone for not being vaccinated; there are many reasons why some are not vaccinated. However, the reality is that, without a vaccination, the risks of COVID-19 infections and further outbreaks are higher.
2. COVID-19 infections are still occurring and, among them, variants such as the Delta Variant are being transmitted; the risk of COVID-19 exposures is not currently low enough that the virus is not circulating among those without vaccinations.
This is important because, with COVID-19 infections still occurring and variants being identified, there is a need for exposure prevention. In analyzing risks, risk levels are only lowered by decreases in the frequency of exposure and the severity of the hazard; risk are not lowered by decreases in incidents resulting from the hazard. For example, when driving a motor vehicle on the freeway at 60 miles per hour, a high risk of a motor vehicle collision exists warranting the use of a seatbelt and defensive driving techniques. Even if a motor vehicle collision has not occurred in a time, this absence of an incident does not remove the risk from driving a motor vehicle at high speeds, so the risk controls (seatbelt and defensive driving) are still necessary. The only way to remove the need for the risk controls is to remove the risk, which means not driving the motor vehicle. With COVID-19, with the virus still existing at variable levels, to lower the actual risk, the virus’s presence needs to be lessened; this is done with vaccinations and/or exposure prevention. However, if vaccines are refused and exposure prevention methods are not enacted, the risk level remains and, if infections still occur, the virus can continue circulating.
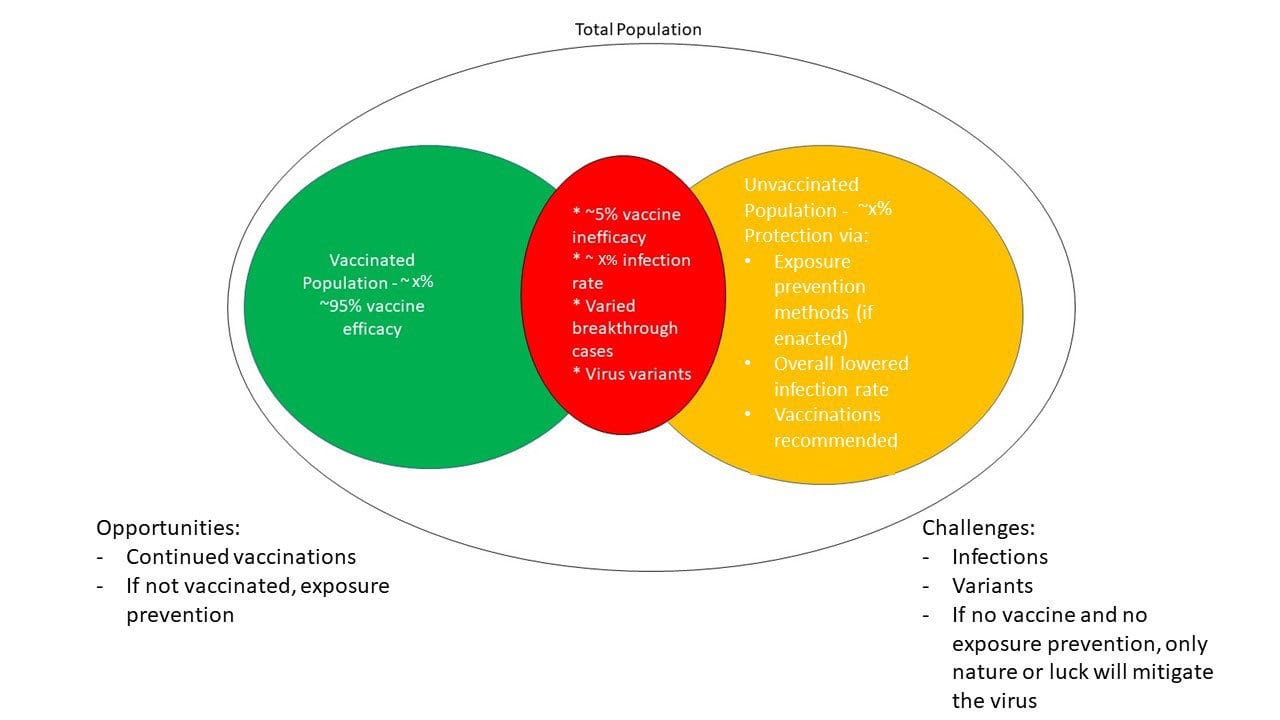
Chart: Cory Worden
A stalemate with the virus
Among the total population, a large percentage has been vaccinated against COVID-19. Among the vaccinated, there is a good level of protection with a small risk of vaccine inefficacy. These vaccinations have created significantly reduced infection rates. However, with the virus still circulating among the unvaccinated and the small vaccine inefficacy risk, it could continue to do so without more vaccinations and/or continued exposure prevention until the actual risk (frequency and severity) is low enough to prevent circulation. But, if the currently unvaccinated do not receive vaccines and do not enact exposure prevention methods, there is no ‘ammunition’ to use against the virus. The virus may only stop circulating through nature or luck. There will be a stalemate. With the valid and reliable means of reducing COVID-19’s risk being vaccinations and exposure prevention methods, protesting both is indirect risk acceptance. With this risk acceptance, others may be placed at risk; this means one person’s risk acceptance can be put on others.
How it happened
With so many protesting vaccinations and exposure prevention protocols, there are several reasons for this. Some have learned to and/or advised others to question and/or refuse vaccinations, face covering policies, COVID-19 testing, social distancing, capacity limits, and other safety protocols. Those without vaccinations who would ideally be donning face covers for source control (droplet containment) and maintaining social distance are likely not doing so; this limits exposure prevention probabilities. This means those who are actively working to prevent COVID-19 exposures through droplet containment (source control) and vaccinations are already doing so and, unfortunately, those who would ideally be practicing exposure prevention if not vaccinated and then pursuing vaccinations are not doing so. More cannot be vaccinated to develop more population immunity if they protest vaccinations and exposures cannot be prevented if they protest methods such as social distancing. In effect, this situation negates the potential opportunity of more vaccinated persons and/or fewer exposures; the level of population immunity and exposure prevention now, from those already having done so, is possibly the most there will be. With this, the COVID-19 risk level is no longer scientifically or statistically correlated to preventative measures for an ideally decreasing risk. Instead, with those protesting vaccinations and exposure prevention, their chosen level of risk acceptance will become society’s.
While those with vaccinations have a good level of protection against COVID-19, the effects of those both unvaccinated and not practicing exposure prevention are that the virus will continue circulating and may affect the vaccinated from the ~5% vaccine inefficacy risk. Prior to the COVID-19 virus reaching the United States, precedents were already known in the forms of Influenza, Tuberculosis, and Ebola, among others. These precedents taught that, even with known exposure prevention controls, these are not entirely reliable if risk acceptance is enabled and if the exposure prevention controls are not utilized in real-time. Even with annual Influenza vaccinations, cases are still known; with exposure prevention protocols such as not entering public spaces while ill, social distancing, source control (droplet containment) if ill, and hand hygiene, many exposures can be prevented, but this exposure prevention has not been normalized in many areas over the years.
Conclusion
Music fans all over the United States noticed a benchmark in May 2021; many bands and their tours — all crowded events with little or no social distancing — that had been abruptly cancelled in 2020 were re-announced to begin in the summer of 2021. Many of them issued press releases stating something to the effect of, ‘This pandemic has not been overcome, but we are going to proceed with our events.’ In essence, they were stating that, there was no real chance of the virus being beaten, so it no longer made sense to keep waiting. They would simply begin scheduling crowded events, proceed with them, and hope for the best. In theory, if people receive vaccinations, the risk can be mitigated, but there are many — approximately half of the country via surveys — who will not commit to them. With no preventative measures — no increased vaccination rates, no higher-effectiveness exposure prevention controls — to apply towards the virus, we, as a world, have reached a stalemate. We can only hope for nature to further lower infection rates. If it happens, it is from luck, good fortune, or a fluke, but not from a valid and reliable method of exposure prevention. Sadly, this sets the precedent for any future pandemics at the same or higher losses as the COVID-19 pandemic because we will not know what could have been regarding prevention. The rhetoric and politization of the COVID-19 response had and will have irreparable consequences on future preventative efforts due to necessary scientific exposure prevention protocols being artificially and politically tainted.
Finally, it is of relevance that, even with a decrease in the COVID-19 infection rate after 18+ months, this is, despite claims that the pandemic was not a high risk and that risk acceptance claims that exposure prevention protocols were never needed, this decrease is due to the combination of exposure prevention and vaccinations put forth by those controlling the risk, despite those denying the risk. The infection rate decrease does not indicate that a high risk never existed. In the future, should another pandemic-level virus appear, a false belief that COVID-19 was not a high risk – when COVID-19 infection rates were mitigated by dutiful efforts in vaccinations and exposure prevention – will again lead to preventable exposures, infections, hospitalizations, and deaths.
Cory Worden, PhD*(ABD), MS, CSHM, CSP, CHSP, ARM, REM, CESCO, AOHP, Region 2 Director, has over 15 years’ experience in safety. He has published six books; his work has been published by ASSP AOHP, ISHN, ISHM and more. Cory was the 2014 ISHM Safety Professional of the Year, a 2015 National Safety Council Rising Star of Safety, the 2016 ASSP Healthcare Practice Specialty Safety Professional of the Year, the 2017 AOHP National Extraordinary Member and the 2018 AOHP Extraordinary Services Award recipient.
NOVEMBER 2021
VOL. 55 NO. 11
