leadership
THOUGHT
By Cory Worden

In this three-part series, the role of personal perceptions and the influence of invalidated information on them used in risk assessments is explored.
Navigating ethical dilemmas
Consider personal perceptions and levels of transparency when assessing risk to improve safety
ith ethical dilemmas facing us every day, these dilemmas create more residual issues. Within ethics, no definite ‘correct’ answer exists; therefore, risk assessments are potential ethical dilemmas — any one person’s opinion or preference can sway or even dictate their outcomes.
The tricky part is knowing when this inherent subjectivity is creating a danger. With no “correct” answer, the question instead becomes, “What is the best of the available ethical options?” With this, perception from team members or the public resulting from this decision also lingers. Will the decision lead them to believe the decision maker has safety in mind or is more concerned with finances, efficiency or another factor(s)?
W
In this situation, transparency is important; if the decision maker(s) cannot articulate how he/she/they came to the risk assessment they did or why they made the risk treatment decision they did, those affected by the decision can easily perceive the leader to be unethical. For an employee to see countless news reports of a pandemic and then see his or her organizational leader(s) claiming no need for distancing, face covers, disinfectants and hand hygiene, the situation is perceived as unethical. Likewise, if employers expect team members to work without hazard controls and then see state and federal leaders develop legislation to give organizational leaders immunity from litigation should a worker become ill without organizational prevention efforts, it can be perceived as unethical.
In the Stankwicks’ Understanding Business Ethics (2009), a myth is identified that companies will operate on the assumption that they have hired employees who are inherently ethical. However, this myth foregoes the fact that each employee’s version of an ethical decision is based on his or her personal perception. This perception can be swayed by personal experience, opinion, politics or other factors. With this, the potential for unethical decisions needs to be controlled through transparency, methodical feedback collection and calculated safety decision making.
In another of the myths identified by the Stanwicks (2009), ethics are driven by compliance standards. However, as previously identified, some hazards, including COVID-19, did not or do not have regulatory standards attached to them. Instead, the implementation of hazard controls is dependent on personal or organizational perceptions that lead to them; these personal perceptions are, as stated in the first myth, dependent on the individual leader being ethical. Lastly, the Stanwicks’ (2009) third myth of ethics in the workplace states that ethics are not considered practical or pragmatic by organizations.
However, without operational safety and necessary hazard controls, the increased risk that comes from this situation raises the probability that an exposure or injury will occur. In the case of COVID-19, this could mean an exposure leading to a confirmed case leading to exponentially more exposures and cases, each of which was preventable had the risk been assessed and controls implemented. However, if the risk assessment claimed the virus to be a low risk based on personal experience, perception, politics or other factors not considering the many variables and factors increasing the risk of the virus existing in the workplace, these exposures will become very practical and pragmatic in short time, functionally stopping operations (Worden, 2020). When ethical dilemmas interfere with proper risk assessments, create gaps in hazard controls or allow for unsafe situations, exposures, injuries and even deaths can occur. This has occurred many times.
Ensuring ethics
With ethical decision making sometimes being the only intervention between an organization with hazard controls and an organization expecting exposures and injuries, ethical development is necessary. In the case of safety and health, this means choosing the safest of available options, especially when no regulatory basis is provided. This, however, can be challenging. If a methodical process is followed using valid and reliable inputs and the systematic, systemic gathering of feedback, it can be done.
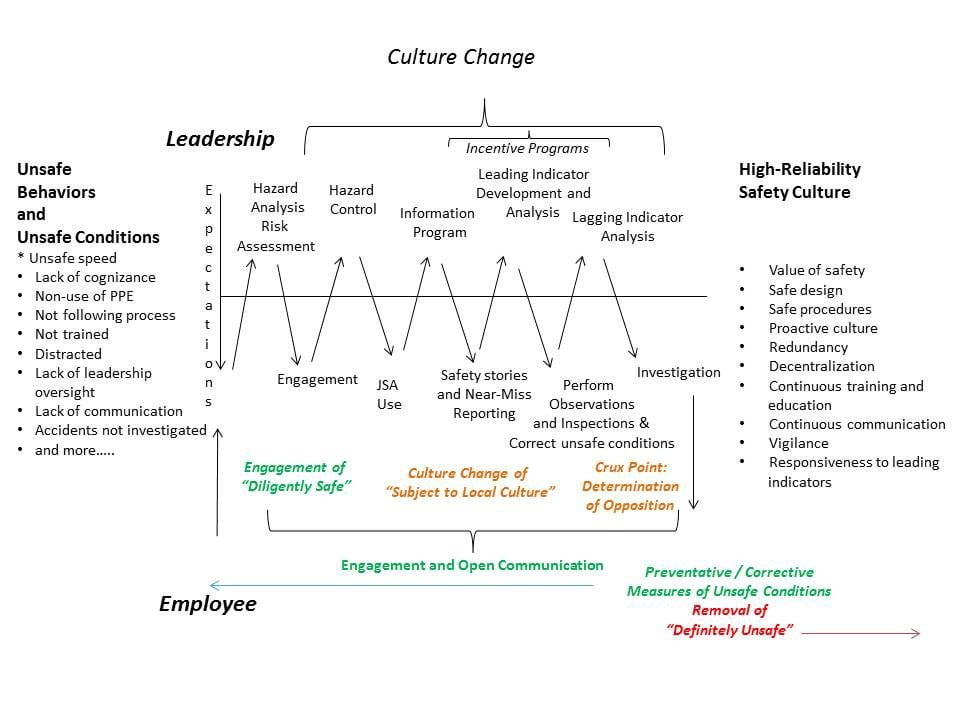
Figure 1: Ethical Workplace Development Courtesy of Cory Worden
Safety committees
Safety Committees are a fundamental fixture in an organizational safety program to develop cross-functional, multi-tiered representation within the teams, lateral communication and managerial support. This can be a guidewire to transformational leadership and uniting a team by allowing for open communication, professional development, share goals and other mutually beneficial cultural aspects between leaders and employees (Rehman & Waheed, 2012). This is also an opportunity for leaders to provide essential professional development opportunities and focus their leadership on the improvement and benefit of their team members for increased servant leadership (Dierendonck, 2011). However, Safety Committees require caution to ensure their support of the employees and avoidance of singular managerial perspectives only accepting inputs benefitting leadership; this can also be the case with union involvement in that unions supporting employees in safety is beneficial while unions covering for unsafe work practices is counterproductive (Weil, 1999).
Hazard identification, risk assessment and hazard control
To ensure ethics, risk assessments must be developed to include objective inputs and data and to develop necessary safety protocols. As discussed earlier in this article, should an organization or government skew a risk assessment to include only subjective perspectives and use this to limit hazard controls, the situation immediately looks unethical. This has been the situation recently with COVID-19 (Lantry & Epps, 2020) and in 2014 with Ebola in Dallas, Texas (Sholchet, 2014). Hazard identifications must include all known information – good, bad and indifferent – about the hazard and who is at risk for exposure. Risk assessments require transparency regarding the frequency and severity of exposure. This information requires timely communication along with action plans for preventing exposures. Hazard control implementations require training for all potentially exposed personnel. Lastly, team feedback is essential to hazard control planning as those doing the work have a clear idea of what is needed.
Communication
Communication of hazard controls and performance expectations needs to be consistent and recurring. Without a clear picture of the hazard, the risk level, the exposure groups, the hazard controls and the expectations, team members cannot be expected to work safely. Any lack of transparency, false information or skewed information will not only put team members at risk but will also create a perception of an unethical work environment.
Additionally, communication is a two-way process. Leaders provide information needed to work safely but employees also provide communication on the status of operations, safety stories, good catch reports and other information aspects to the communication effort. This two-way communication also provides a valuable opportunity to help remove any disinformation being discussed in the workplace whether from leaders or team members. Culturally, without communication, it is very easy for team members to perceive unethical leadership as they would not hear about safety and possibly assume it is not a factor in their leadership’s management of the team.
Leading indicators
Leading indicators to validate safe working conditions and safe work practices are imperative. Regardless of hazard controls and communication, if those elements are not validated during operations, safety is just based on luck. For example, if team members are expected to don a respirator prior to entering a contaminated area, this requires real-time observations to ensure the donning takes place, the respirator can be sealed, the same respirator is being used operationally that was used to pass the Fit Test, the respirator is doffed without cross-contamination and more.
With these leading indicators, good catch reports can be enabled to continually improve operations and recognition programs for positive reinforcement can be developed to build continued safety. Culturally, leading indicators provide validation of operational safety and allow team members an opportunity to voice concerns. This is important in that an ethical workplace allows for transparent, lateral communication to remove any perceptions that impropriety is taking place. Furthermore, this allows for more, better inputs to the risk assessment to further remove subjectivity.
Lagging Indicators and Investigations
Lagging indicators provide data and measurements as to exposures and injuries that have occurred. While this information is only serving to identify what has already gone wrong, it provides information as to the frequency and severity of the hazard so that the risk assessment can be updated and also provides analysis opportunities to determine preventative and corrective measures to continually improve processes. Culturally, lagging indicators provide more indicators for analysis to increase the objectivity of the risk assessment and offer more transparency, another indicator of an ethical workplace. However, caution is needed with lagging indicators to prevent any HIPAA violations.
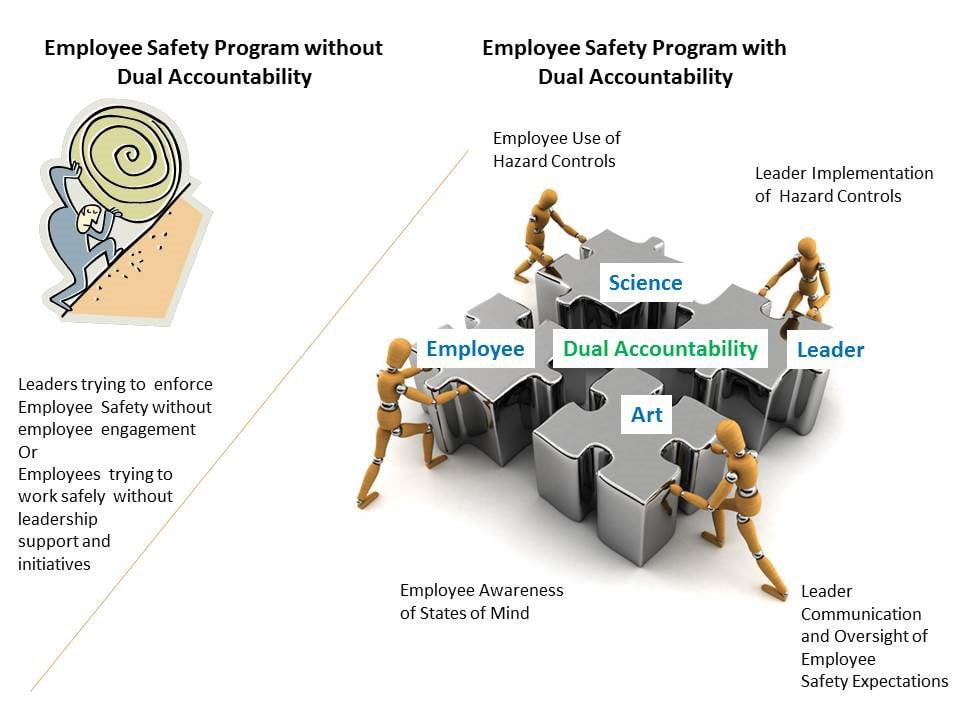
Figure 2: Dual Accountability Courtesy of Cory Worden
Dual accountability
As shown by the development of the safety program, every component from the Safety Committee makeup to the risk assessment to the leading and lagging indicators requires checks and balances through valid, reliable information, transparent communication and participation from all tiers and functionalities. With this, dual accountability is required. Leaders are certainly required to identify hazards, assess risk and implement hazard controls. However, team members are then required to participate in these processes and to actively and properly follow the protocols. Leaders are required to validate safety during operations while team members are required to participate and follow the protocols. Neither can be exempt from safety and neither can point to the other as a reason or rationale for safety being valued within the team.
Conclusion
Everything varied about COVID-19’s safety protocols began with its risk assessment. Some leaders selectively chose data to confirm their desired narrative. Some leaders selectively chose words to underrepresent the hazard and risk. Some leaders communicated data points showing the frequency – test cases and severity, hospitalizations and other medical data – but that data was itself convoluted by varied messages about what it represented. With a subjective risk assessment based on perceptions and personal experiences and politics, hazard control implementations can, and did, become subject to somebody’s chosen assessment instead of a science-based necessity. Ultimately, this can leave people without protection or useful knowledge because somebody else did not believe it was necessary.
Sadly, COVID-19 is not the first time this phenomenon has occurred. It occurred in 2014 with Ebola in terms of preparedness with hospitals scrambling to learn highly infectious patient protocols after the virus made its way to the United States and after one hospital found itself with an infectious patient, exposed team members and piles of hazardous waste with no way to dispose of it. It happened in the 1960s with the Vietnam War when politicians handpicked their narrative to promulgate the war knowing it would mean sending more service members to fight it (Ellsberg, 2002).
It happened in the 2000s when politicians handpicked a narrative falsely showing Weapons of Mass Destruction in Iraq to promulgate a war there knowing it would mean sending more service members to fight it (Gordon & Trainer, 2007). It has happened in workplaces with heavy equipment where leaders subjectively perceived the risk as ‘low’, but their untrained employees were later killed by the same hazard the leaders deemed ‘low risk’ (Worden, 2015).
For this to stop happening, holistic team efforts are needed for hazard identifications and risk assessments using objective, valid and reliable data. With the risk assessed, transparent communication and open validation of safety protocols are needed. Transparent, lateral communication of safety incidents (without HIPAA violations) and team efforts for continual improvements are needed. With these safety developments and removals of subjective, personal perception-driven risk assessment leading to exposed employees, safety can be dramatically improved, and catastrophes can be prevented. This is the way to high reliability operations.
Cory Worden, PhD*(ABD), MS, CSHM, CSP, CHSP, ARM, REM, CESCO, AOHP, Region 2 Director, has over 15 years’ experience in safety. He has published six books; his work has been published by ASSP AOHP, ISHN, ISHM and more. Cory was the 2014 ISHM Safety Professional of the Year, a 2015 National Safety Council Rising Star of Safety, the 2016 ASSP Healthcare Practice Specialty Safety Professional of the Year, the 2017 AOHP National Extraordinary Member and the 2018 AOHP Extraordinary Services Award recipient.
JUNE 2021
VOL. 55 NO. 6